Overview & Why Choose Dr. Chang
Skin cancer is the most common type of cancer in the United States. In addition to removing the cancer to prevent potentially life-threatening consequences, it is incredibly important for the surgeon to aesthetically and functionally reconstruct the defect left behind. Whether you have been diagnosed with basal cell carcinoma, squamous cell carcinoma, or melanoma on the face, body, or extremities, Dr. Chang understands the profound psychological and social effects skin cancer may have. He is committed to addressing these concerns with sensitivity and expertise. His goal is to restore not only the form but also the function of your face, body, or extremity, ensuring that your appearance is as natural and inconspicuous as possible.
Dr. Chang’s extensive experience and compassionate approach are key to achieving excellent outcomes.
Many of these procedures can be performed comfortably under local anesthesia in his office, allowing for a more convenient and less invasive treatment experience. His meticulous technique focuses on preserving facial aesthetics and function, hiding your scars in natural facial transition zones and shadows. Dr. Chang will work closely with you to understand your goals and expectations. By combining advanced surgical techniques with personalized care, Dr. Chang aims to deliver results that restore your confidence and quality of life, helping you to move forward with renewed self-assurance.
Types of Conditions Treated
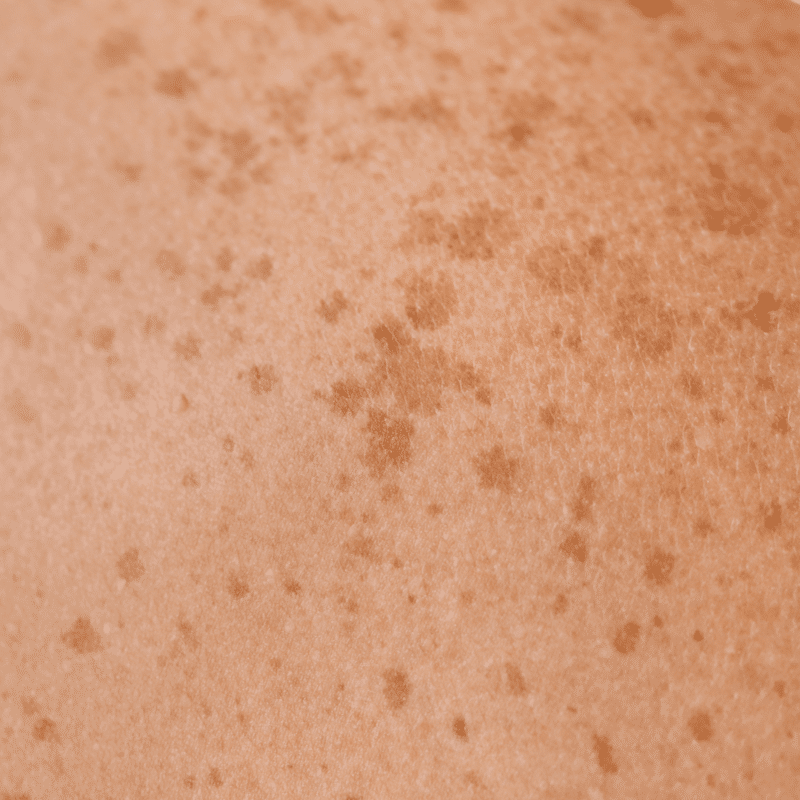
- Basal Cell Carcinoma (BCC) is the most frequently diagnosed skin cancer, accounting for about 80% of all non-melanoma skin cancers. It often appears as a small, pearly bump or a pinkish growth, primarily on sun-exposed areas such as the face, ears, neck, and back.
- Squamous Cell Carcinoma (SCC) is the second most common type, comprising approximately 20% of non-melanoma skin cancers. SCC typically manifests as a red, scaly patch or a sore that doesn’t heal, commonly found on the face, ears, lips, and backs of hands.
- Melanoma is less common but more aggressive, responsible for about 1% of all skin cancer cases. It usually presents as a new or changing mole, characterized by asymmetry, irregular borders, varied colors, or an increase in size. Melanoma can develop anywhere on the body but is most frequently found on the back, legs, arms, and face.
- Merkel Cell Carcinoma (MCC) is a rare but highly aggressive form of skin cancer. It appears as a painless, firm, and rapidly growing nodule, often on sun-exposed areas such as the head, neck, or limbs. MCC is known for its tendency to spread quickly to other parts of the body.
- Sebaceous Gland Carcinoma is an uncommon and aggressive cancer arising from the oil glands in the skin. It can present as a hard, painless lump or a nodule with a yellowish hue, typically found on the eyelids, scalp, or face.

Pre-Operative
- Biopsy – A biopsy is crucial for any lesion highly suspicious for cancer, as it provides definitive confirmation of the cancer type and informs the surgical planning. By analyzing a small sample of the lesion, we can accurately map the extent of the cancer and determine the most effective approach for its removal.
- Diagnostic Imaging – Depending on the type of skin cancer, additional diagnostics or procedures may be necessary to check for any cancer spread.
- Medical Evaluation – Depending on the planned resection and reconstruction, you may require a comprehensive medical evaluation if general anesthesia is needed. This evaluation ensures that any underlying health conditions are managed appropriately and that you are in optimal condition for a safe surgical experience.
Technique
- Skin Cancer Resection – Skin cancer resection involves the precise removal of both the cancerous lesion and a margin of healthy skin surrounding it, as well as some of the fat beneath the skin. This margin is crucial to minimize the risk of local recurrence, as cancer cells can extend beyond the visible edges of the tumor. Consequently, the area of skin removed is often significantly larger than the original cancerous lesion. For facial lesions, this can be particularly challenging, requiring a delicate balance between ensuring complete cancer removal and preserving cosmetic appearance. In some cases, Mohs micrographic surgery by a dermatologist may be recommended to precisely remove cancerous cells, followed by reconstruction. The tissue removed will be carefully assessed and marked for final pathology to confirm that all cancerous cells have been removed.
- Reconstruction by Primary Closure – Small resections in areas where the skin can be easily pulled together without distorting the surrounding tissues can be treated by directly suturing the skin edges together.
- Reconstruction with Skin Grafts – Skin is borrowed from one part of your body and sutured over the wound created by the resection. This is a good option for larger defects in patients who would like to avoid additional scars from local flaps. The downside is there may be a noticeable difference in texture and color between the graft and surrounding skin. The part of the body where the skin is borrowed from is sutured together primarily.
- Reconstruction with Local Flaps – Local flaps are the most common method of reconstructing skin cancer wounds on the face. Local flaps use nearby skin and tissue to reconstruct the area. Although multiple incisions are made, they are carefully placed in natural facial transition zones to minimize visible scarring. Local flaps are particularly beneficial for facial reconstructions due to their superior match in skin color, texture, and thickness. There are many, many types of local flaps that can be used all over the body, particularly the face. Dr. Chang’s extensive knowledge of these flaps allows him to choose the ones that will best reconstruct your specific wound while minimizing visible scarring.
- Reconstruction with Distant Flaps – Used for more severe cases where local tissue is insufficient. These flaps involve transferring tissue from a distant site, which requires additional surgical steps and has a longer recovery time.
- Single-Stage versus Multiple-Stage Reconstruction – For many skin cancers, they can be resected and reconstructed in a single procedure in the same clinic visit. For more complex skin cancers, especially ones that involve a more 3D structure, such as the nose, ears, or lips, a multiple-stage approach can be better. By separating certain goals and steps of the reconstruction into distinct procedures, you can have the most natural and optimal long-term result.
- Cartilage Grafting – Resection of skin cancers involving structures such as the nose or ears may result in more noticeable structural defects. To give back the 3D support of the native structure, cartilage from your nose, ear, or rib may be needed to achieve the best result.
Anesthesia
- Local Anesthesia – For small skin cancers that need more routine reconstruction techniques, the procedure can be performed under local anesthesia in the office.
- General Anesthesia – For more complex skin cancers that require more advanced reconstruction techniques, Dr. Chang may recommend that the procedure be performed in the operating room under general anesthesia.
Post-Operative
- Dressings and Incision Care – Your incisions will be sutured with absorbable or permanent sutures. For skin cancers involving the face, the incisions will be covered with antibiotic ointment and a gauze bandage to help with any oozing for the first 24 hours. Thereafter, you may leave the incisions open to air with the antibiotic ointment or apply a bandage as you desire. For skin cancers involving the body or extremities, you will likely have surgical bandage strips. You may shower the day after surgery but cannot bathe or swim until instructed to do so.
- Neurotoxin for Scar Management – Depending on the location of your incisions, you may benefit from neurotoxin injections to help optimize the final appearance of the scar to make it as imperceptible as possible. By limiting the movement of the muscles and overlying skin near the incisions, the neurotoxin limits the stress and movement on the final scar.
- Pain Management and Medications – Local anesthetic (numbing medication) will be injected at your surgical sites to minimize your immediate post-operative pain. You should take acetaminophen and an NSAID around-the-clock, according to instruction, for the first 72 hours and then as-needed thereafter. You can purchase these over-the-counter. For more complex procedures, you will be given a small number of low-dose narcotic pain medications for breakthrough pain only for the first 72 hours.
- Recovery Period – You are expected to go home the same day of surgery and should be ambulating without restriction the same day of surgery. You should expect some drainage from the incisions and mild bruising around the incisions. You will be swollen, and it can take up to 3-6 months for the swelling to reside. Your incisions will take 2-4 weeks to completely heal, but the final scar will take 6-12 months to mature. Scar care will be discussed at your 1 month post-operative appointment.
- Follow-Up Visits – If you have any urgent concerns, you may call the office at any time. Otherwise, expect follow-up visits at 1 week, 1 month, 3 months, 6 months, and 1 year.
Complications
- Incomplete Cancer Resection and Need for Re-Excision – Sometimes, the initial resection may not achieve clear margins, requiring additional surgery to ensure that all cancerous cells have been removed.
- Skin Cancer Recurrence – Even with a thorough resection, there is a possibility of the cancer returning. Regular follow-up appointments and surveillance are crucial in monitoring for any signs of recurrence.
- Development of Skin Cancer in a Separate Location – While the primary cancer may be removed successfully, new skin cancers can develop in other areas, especially if there is a history of extensive sun exposure or other risk factors. Routine skin examinations and preventive measures are recommended to reduce the risk of new cancers forming.
- Poor Scarring – Everyone scars differently. The final scar takes 6-12 months to mature. In rare cases, hypertrophic scars or keloids may form and may require secondary revision.
- Wound Healing Issues – There may be small areas where the incisions do not fully heal. In these cases, the wounds will be allowed to heal on their own with dressing changes. Severe cases may require a secondary revision procedure.
- Infection – Infections are managed with antibiotics. In severe cases, you may need an additional procedure.
- Unmet Expectations – Despite thorough pre-operative planning and discussions, you still may not be fully happy with your aesthetic results. Skin cancers that require extensive resection on the face will distort your normal facial anatomy. While the goal of reconstruction is to minimize the noticeable sequelae of the cancer, your face will not be exactly the same it was before surgery.